J u m p t o c o n t e n t
M a i n m e n u
M a i n m e n u
N a v i g a t i o n
● M a i n p a g e ● C o n t e n t s ● C u r r e n t e v e n t s ● R a n d o m a r t i c l e ● A b o u t W i k i p e d i a ● C o n t a c t u s ● D o n a t e
C o n t r i b u t e
● H e l p ● L e a r n t o e d i t ● C o m m u n i t y p o r t a l ● R e c e n t c h a n g e s ● U p l o a d f i l e
S e a r c h
Search
A p p e a r a n c e
● C r e a t e a c c o u n t ● L o g i n
P e r s o n a l t o o l s
● C r e a t e a c c o u n t ● L o g i n
P a g e s f o r l o g g e d o u t e d i t o r s l e a r n m o r e ● C o n t r i b u t i o n s ● T a l k
( T o p )
1 S i g n s a n d s y m p t o m s
2 C a u s e s
T o g g l e C a u s e s s u b s e c t i o n
2 . 1 A s s o c i a t i o n s
3 T y p e s
4 T r e a t m e n t
5 E p i d e m i o l o g y
6 R e f e r e n c e s
T o g g l e t h e t a b l e o f c o n t e n t s
U t e r i n e i n v e r s i o n
1 1 l a n g u a g e s
● ا ل ع ر ب ي ة ● E s p a ñ o l ● F r a n ç a i s ● B a h a s a I n d o n e s i a ● I t a l i a n o ● ע ב ר י ת ● മ ല യ ാ ള ം ● ଓ ଡ ଼ ି ଆ ● P o l s k i ● P o r t u g u ê s ● Р у с с к и й
E d i t l i n k s
● A r t i c l e ● T a l k
E n g l i s h
● R e a d ● E d i t ● V i e w h i s t o r y
T o o l s
T o o l s
A c t i o n s
● R e a d ● E d i t ● V i e w h i s t o r y
G e n e r a l
● W h a t l i n k s h e r e ● R e l a t e d c h a n g e s ● U p l o a d f i l e ● S p e c i a l p a g e s ● P e r m a n e n t l i n k ● P a g e i n f o r m a t i o n ● C i t e t h i s p a g e ● G e t s h o r t e n e d U R L ● D o w n l o a d Q R c o d e ● W i k i d a t a i t e m
P r i n t / e x p o r t
● D o w n l o a d a s P D F ● P r i n t a b l e v e r s i o n
I n o t h e r p r o j e c t s
● W i k i m e d i a C o m m o n s
A p p e a r a n c e
F r o m W i k i p e d i a , t h e f r e e e n c y c l o p e d i a
Uterine inversion Complete inverted uterus Specialty Obstetrics Symptoms Postpartum bleeding , abdominal pain, mass in the vagina, low blood pressure [1] Types First, second, third, fourth degree[1] Risk factors Pulling on the umbilical cord or pushing on the top of the uterus before the placenta has detached, uterine atony , placenta previa , connective tissue disorders [1] Diagnostic method Seeing the inside of the uterus in the vagina[2] Differential diagnosis Uterine fibroid , uterine atony , bleeding disorder , retained placenta [1] Treatment Standard resuscitation , rapidly replacing the uterus[1] Medication Oxytocin , antibiotics [1] Prognosis ~15% risk of death[3] Frequency About 1 in 6,000 deliveries[1] [4]
Uterine inversion is when the uterus turns inside out, usually following childbirth .[1] postpartum bleeding , abdominal pain, a mass in the vagina, and low blood pressure .[1] pregnancy .[5]
Risk factors include pulling on the umbilical cord or pushing on the top of the uterus before the placenta has detached.[1] uterine atony , placenta previa , and connective tissue disorders .[1] vagina .[2] [6]
Treatment involves standard resuscitation together with replacing the uterus as rapidly as possible.[1] [1] oxytocin and antibiotics are typically recommended.[1] [1]
Uterine inversion occurs in about 1 in 2,000 to 1 in 10,000 deliveries.[1] [4] developing world .[1] [3] [1] Hippocrates .[1]
Signs and symptoms
[ edit ] Drawing of an inverted uterus
Uterine inversion is often associated with significant postpartum bleeding . Traditionally it was thought that it presented with haemodynamic shock "out of proportion" with blood loss, however blood loss has often been underestimated. The parasympathetic effect of traction on the uterine ligaments may cause bradycardia .
Causes
[ edit ]
The most common cause is the mismanagement of 3rd stage of labor, such as:
Fundal pressure
Excess cord traction during the 3rd stage of labor
Other natural causes can be:
Uterine weakness, congenital or not
Precipitate delivery
Short umbilical cord
It is more common in multiple gestation than in singleton pregnancies.
Associations
[ edit ]
Types
[ edit ] Incomplete (left) and complete (right) inversion of the uterus
One: Complete. Visible outside the cervix .
Two: Incomplete. Visible only at the cervix.[7]
Treatment
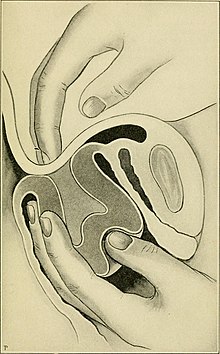
[ edit ] Manual replacement of the uterus
Treatment involves standard resuscitation together with replacing the uterus as rapidly as possible.[1] [1] oxytocin and antibiotics are typically recommended.[1] [1]
Epidemiology
[ edit ]
Uterine inversion occurs in about 1 in 2,000 to 1 in 10,000 deliveries.[1] [4] developing world .[1]
References
[ edit ]
^ a b Mirza, FG; Gaddipati, S (April 2009). "Obstetric emergencies". Seminars in Perinatology . 33 2 ): 97–103. doi :10.1053/j.semperi.2009.01.003 . PMID 19324238 .
^ a b Gandhi, Alpesh; Malhotra, Narendra; Malhotra, Jaideep; Gupta, Nidhi; Bora, Neharika Malhotra (2016). Principles of Critical Care in Obstetrics ISBN 9788132226925
^ a b c Andersen, H. Frank; Hopkins, Michael P. (2009). "Postpartum Hemorrhage". The Global Library of Women's Medicine . doi :10.3843/GLOWM.10138 .
^ Mehra, R; Siwatch, S; Arora, S; Kundu, R (12 December 2013). "Non-puerperal uterine inversion caused by malignant mixed mullerian sarcoma" . BMJ Case Reports . 2013 : bcr2013200578. doi :10.1136/bcr-2013-200578 . PMC 3863018 PMID 24334469 .
^ Apuzzio, Joseph J.; Vintzileos, Anthony M.; Berghella, Vincenzo; Alvarez-Perez, Jesus R. (2017). Operative Obstetrics, 4E ISBN 9781498720588
^ Uterine inversion Archived 2009-10-04 at the Wayback Machine - Better Health Channel; State of Victoria, Australia; accessed 2009-04-03
R e t r i e v e d f r o m " https://en.wikipedia.org/w/index.php?title=Uterine_inversion&oldid=1216394354 " C a t e g o r y : ● C o m p l i c a t i o n s o f l a b o u r a n d d e l i v e r y H i d d e n c a t e g o r i e s : ● W e b a r c h i v e t e m p l a t e w a y b a c k l i n k s ● A r t i c l e s w i t h s h o r t d e s c r i p t i o n ● S h o r t d e s c r i p t i o n i s d i f f e r e n t f r o m W i k i d a t a ● W i k i p e d i a m e d i c i n e a r t i c l e s r e a d y t o t r a n s l a t e
● T h i s p a g e w a s l a s t e d i t e d o n 3 0 M a r c h 2 0 2 4 , a t 1 8 : 5 4 ( U T C ) . ● T e x t i s a v a i l a b l e u n d e r t h e C r e a t i v e C o m m o n s A t t r i b u t i o n - S h a r e A l i k e L i c e n s e 4 . 0 ;
a d d i t i o n a l t e r m s m a y a p p l y . B y u s i n g t h i s s i t e , y o u a g r e e t o t h e T e r m s o f U s e a n d P r i v a c y P o l i c y . W i k i p e d i a ® i s a r e g i s t e r e d t r a d e m a r k o f t h e W i k i m e d i a F o u n d a t i o n , I n c . , a n o n - p r o f i t o r g a n i z a t i o n . ● P r i v a c y p o l i c y ● A b o u t W i k i p e d i a ● D i s c l a i m e r s ● C o n t a c t W i k i p e d i a ● C o d e o f C o n d u c t ● D e v e l o p e r s ● S t a t i s t i c s ● C o o k i e s t a t e m e n t ● M o b i l e v i e w