J u m p t o c o n t e n t
M a i n m e n u
M a i n m e n u
N a v i g a t i o n
● M a i n p a g e ● C o n t e n t s ● C u r r e n t e v e n t s ● R a n d o m a r t i c l e ● A b o u t W i k i p e d i a ● C o n t a c t u s ● D o n a t e
C o n t r i b u t e
● H e l p ● L e a r n t o e d i t ● C o m m u n i t y p o r t a l ● R e c e n t c h a n g e s ● U p l o a d f i l e
S e a r c h
Search
A p p e a r a n c e
● C r e a t e a c c o u n t ● L o g i n
P e r s o n a l t o o l s
● C r e a t e a c c o u n t ● L o g i n
P a g e s f o r l o g g e d o u t e d i t o r s l e a r n m o r e ● C o n t r i b u t i o n s ● T a l k
( T o p )
1 C a u s e s
T o g g l e C a u s e s s u b s e c t i o n
1 . 1 L i s t o f c a u s e s
2 M e c h a n i s m
3 D i a g n o s i s
4 T r e a t m e n t
5 S e e a l s o
6 R e f e r e n c e s
7 F u r t h e r r e a d i n g
8 E x t e r n a l l i n k s
T o g g l e t h e t a b l e o f c o n t e n t s
P o l y u r i a
3 1 l a n g u a g e s
● ا ل ع ر ب ي ة ● C a t a l à ● Č e š t i n a ● D e u t s c h ● E s p a ñ o l ● E u s k a r a ● ف ا ر س ی ● F r a n ç a i s ● 한 국 어 ● Հ ա յ ե ր ե ն ● H r v a t s k i ● B a h a s a I n d o n e s i a ● I t a l i a n o ● N e d e r l a n d s ● N o r s k b o k m å l ● P o l s k i ● P o r t u g u ê s ● Р у с с к и й ● S h q i p ● س ن ڌ ي ● S l o v e n š č i n a ● ک و ر د ی ● С р п с к и / s r p s k i ● S u o m i ● S v e n s k a ● த ம ி ழ ் ● T ü r k ç e ● У к р а ї н с ь к а ● T i ế n g V i ệ t ● 粵 語 ● 中 文
E d i t l i n k s
● A r t i c l e ● T a l k
E n g l i s h
● R e a d ● E d i t ● V i e w h i s t o r y
T o o l s
T o o l s
A c t i o n s
● R e a d ● E d i t ● V i e w h i s t o r y
G e n e r a l
● W h a t l i n k s h e r e ● R e l a t e d c h a n g e s ● U p l o a d f i l e ● S p e c i a l p a g e s ● P e r m a n e n t l i n k ● P a g e i n f o r m a t i o n ● C i t e t h i s p a g e ● G e t s h o r t e n e d U R L ● D o w n l o a d Q R c o d e ● W i k i d a t a i t e m
P r i n t / e x p o r t
● D o w n l o a d a s P D F ● P r i n t a b l e v e r s i o n
A p p e a r a n c e
F r o m W i k i p e d i a , t h e f r e e e n c y c l o p e d i a
Medical condition
Polyuria () is excessive or an abnormally large production or passage of urine (greater than 2.5 L[1] [6] diuresis .[7] [8] polydipsia (increased thirst), though it is possible to have one without the other, and the latter may be a cause or an effect. Primary polydipsia may lead to polyuria.[9] symptom or sign of another disorder (not a disease by itself), but it can be classed as a disorder, at least when its underlying causes are not clear.[citation needed
Causes
[ edit ]
The most common cause of polyuria in both adults and children is uncontrolled diabetes mellitus ,[6] osmotic diuresis ; when glucose levels are so high that glucose is excreted in the urine. Water follows the glucose concentration passively, leading to abnormally high urine output. In the absence of diabetes mellitus, the most common causes are the decreased secretion of aldosterone due to adrenal cortical tumor, primary polydipsia (excessive fluid drinking ), central diabetes insipidus , and nephrogenic diabetes insipidus .[6] diuretics , caffeine , and ethanol . It may also occur after supraventricular tachycardias , during an onset of atrial fibrillation , childbirth , and the removal of an obstruction within the urinary tract . Diuresis is controlled by antidiuretics such as vasopressin , angiotensin II and aldosterone . Cold diuresis is the occurrence of increased urine production upon exposure to cold, which also partially explains immersion diuresis . High-altitude diuresis occurs at altitudes above 10,000 feet (3,000 m ) and is a desirable indicator of adaptation to high altitudes . Mountaineers who are adapting well to high altitudes experience this type of diuresis. People who produce less urine even in the presence of adequate fluid intake are probably not adapting well to high altitudes.[10]
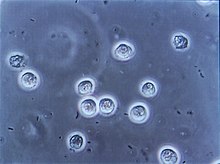
Urinary tract infection (bacteria are black and bean-shaped)
List of causes
[ edit ] Emphysematous cystitis Lithium-carbonate
psychogenic polydipsia [2]
diuretic drugs, osmotic diuresis [11]
Urinary system
Hormonal
Circulation
Neurologic
Other
Mechanism
[ edit ]
Polyuria, in osmotic cases, increases flow amount in the distal nephron where flow rates and velocity are low. The significant pressure increase occurring in the distal nephron takes place particularly in the cortical-collecting ducts. One study from 2008 laid out a hypothesis that hyperglycaemic and osmotic polyuria play roles ultimately in diabetic nephropathy.[40]
Diagnosis
[ edit ]
Among the possible tests to diagnose polyuria are:[4]
FBC
Blood test
Pituitary function test
Treatment
[ edit ]
Depending on the cause of the polyuria, the adequate treatment should be afforded. According to NICE , desmopressin can be considered for nocturnal polyuria, which can be caused by diabetes mellitus,[5] [41]
See also
[ edit ]
References
[ edit ]
^ a b Rippe, editors, Richard S. Irwin, James M. (2008). Irwin and Rippe's intensive care medicine ISBN 978-0-7817-9153-3 . Retrieved 5 August 2015 . CS1 maint: multiple names: authors list (link )
^ a b "Polyuria. Medical Professional reference for Polyuria. | Patient" . Patient . Retrieved 2015-11-08 .
^ a b Merseburger, Axel S.; Kuczyk, Markus A.; Moul, Judd W. (2014-10-21). Urology at a Glance ISBN 9783642548598
^ a b c "Polyuria" . Merck Manuals . November 2013. Retrieved 30 December 2014 .
^ "Definition of Diuresis" . MedTerms . 30 October 2013. Retrieved 30 December 2014 .
^ "Diuresis" . The Free Dictionary . Retrieved 30 December 2014 .
^ Parthasarathy, A. (2014-04-30). Case Scenarios in Pediatric and Adolescent Practice ISBN 9789351520931
^ Research, Institute of Medicine (US ) Committee on Military Nutrition; Marriott, Bernadette M.; Carlson, Sydne J. (1996), "Fluid Metabolism at High Altitudes" , Nutritional Needs In Cold And In High-Altitude Environments: Applications for Military Personnel in Field Operations , National Academies Press (US ), retrieved 2024-03-04
^ Ronco, Claudio (2009). Critical Care Nephrology ISBN 978-1416042525 . Retrieved 5 August 2015 .
^ Paulman, Paul (2012). Signs and Symptoms in Family Medicine: A Literature-Based Approach ISBN 978-0323081320 . Retrieved 5 August 2015 .
^ Drake, edited by Michael Glynn, William M. (2012). Hutchison's clinical methods : an integrated approach to clinical practice ISBN 978-0-7020-4091-7 . Retrieved 5 August 2015 . CS1 maint: multiple names: authors list (link )
^ Lee, [edited by] Mary (2013). Basic skills in interpreting laboratory data ISBN 978-1-58528-343-9 . Retrieved 5 August 2015 .
^ Weissman, [edited by] Barbara N. (2009). Imaging of arthritis and metabolic bone disease ISBN 978-0-323-04177-5 . Retrieved 5 August 2015 .
^ Radiology illustrated : pediatric radiology ISBN 978-3-642-35572-1 . Retrieved 6 August 2015 .
^ Chihan, Nina (2007). Nursing Interpreting Signs and Symptoms ISBN 9781582556680 . Retrieved 5 August 2015 .
^ Brickell, [edited by] Wendy Arneson, Jean (2007). Clinical chemistry : a laboratory perspective ISBN 978-0-8036-1498-7 . Retrieved 5 August 2015 . CS1 maint: multiple names: authors list (link )
^ Soni, Andrew Bersten, Neil (2013). Oh's Intensive Care Manual ISBN 978-0-7020-4762-6 . Retrieved 6 August 2015 . {{cite book }}: CS1 maint: multiple names: authors list (link )
^ "Pediatric Pheochromocytoma Clinical Presentation" . Medscape.com . eMedicine. Retrieved 6 August 2015 .
^ Ghosh, Srinanda (2007). MCQ's in medical surgical nursing : (with explanatory answers) P ) Ltd. p. 150. ISBN 978-81-8448-104-4 . Retrieved 6 August 2015 .
^ Loscalzo, edited by Ajay K. Singh, Joseph (2014). The Brigham intensive review of internal medicine ISBN 978-0-19-935828-1 . Retrieved 6 August 2015 . CS1 maint: multiple names: authors list (link )
^ Acute medicine 201415 ISBN 978-1-907904-25-7 . Retrieved 6 August 2015 .
^ Mariani, Laura (2007). "The Renal Manifestations of Thyroid Disease" . Journal of the American Society of Nephrology . 23 1 ): 22–26. doi :10.1681/ASN.2010070766 PMID 22021708 . Retrieved 6 August 2015 .
^ "Panhypopituitarism Clinical Presentation" . Medscape.com . eMedicine. Retrieved 6 August 2015 .
^ Kost, Michael (2004). Moderate sedation/analgesia : core competencies for practice ISBN 978-0-7216-0324-7 . Retrieved 6 August 2015 .
^ Schwartz, M. William Schwartz; et al., eds. (2012). The 5-minute pediatric consult ISBN 978-1-4511-1656-4 . Retrieved 6 August 2015 .
^ Abrams, Paul (2006). Urodynamics ISBN 978-1-85233-924-1 . Retrieved 6 August 2015 .
^ Leslie, Shern L. Chew, David (2006). Clinical endocrinology and diabetes ISBN 978-0443073038 {{cite book }}: CS1 maint: multiple names: authors list (link )
^ Pavord, Sherif Gonem; foreword by Ian (2010). Diagnosis in acute medicine ISBN 978-184619-433-7 . Retrieved 6 August 2015 . {{cite book }}: CS1 maint: multiple names: authors list (link )
^ Shanley, edited by Derek S. Wheeler, Hector R. Wong, Thomas P. (2014). A Systems Approach ISBN 978-1-4471-6355-8 . Retrieved 6 August 2015 . CS1 maint: multiple names: authors list (link )
^ Parker, Rolland S. (2012). Concussive brain trauma neurobehavioral impairment and maladaptation ISBN 978-1-4200-0798-5 . Retrieved 6 August 2015 .
^ "Migraine Headache Clinical Presentation" . Medscape.com . eMedicine. Retrieved 6 August 2015 .
^ McKee, Mitchell Bebel Stargrove, Jonathan Treasure, Dwight L. (2008). Herb, nutrient, and drug interactions : clinical implications and therapeutic strategies ISBN 978-0-323-02964-3 . Retrieved 6 August 2015 . {{cite book }}: CS1 maint: multiple names: authors list (link )
^ Watkins, edited by W. Allan Walker, John B. (1997). Nutrition in pediatrics : basic science and clinical application ISBN 978-1-55009-026-0 . Retrieved 6 August 2015 . CS1 maint: multiple names: authors list (link )
^ Swienton, editors, Richard B. Schwartz, John G. McManus Jr., Raymond E. (2008). Tactical emergency medicine ISBN 978-0-7817-7332-4 . Retrieved 6 August 2015 . CS1 maint: multiple names: authors list (link )
^ Vyas, JN (2008). Textbook of Postgraduate Psychiatry (2 Vols.) ISBN 978-81-7179-648-9 . Retrieved 6 August 2015 .
^ "Hemochromatosis Clinical Presentation" . Medscape.com . eMedicine. Retrieved 6 August 2015 .
^ J. W. Bennett; M. Klich (2003). "Mycotoxins" . Clin Microbiol Rev . 16 3 ): 497–516. doi :10.1128/CMR.16.3.497-516.2003 . PMC 164220 PMID 12857779 .
^ Wang, Shinong; Mitu, Grace M.; Hirschberg, Raimund (2008-07-01). "Osmotic polyuria: an overlooked mechanism in diabetic nephropathy" . Nephrology Dialysis Transplantation . 23 7 ): 2167–2172. doi :10.1093/ndt/gfn115 ISSN 0931-0509 . PMID 18456680 .
^ "Nocturia and nocturnal polyuria in men with lower urinary tract symptoms: oral desmopressin | key-points-from-the-evidence | Advice | NICE" . www.nice.org.uk . Retrieved 2015-08-03 .
Further reading
[ edit ]
External links
[ edit ]
R e t r i e v e d f r o m " https://en.wikipedia.org/w/index.php?title=Polyuria&oldid=1215549609 " C a t e g o r i e s : ● S y m p t o m s a n d s i g n s : U r i n a r y s y s t e m ● H e a l t h H i d d e n c a t e g o r i e s : ● C S 1 e r r o r s : g e n e r i c n a m e ● C S 1 m a i n t : m u l t i p l e n a m e s : a u t h o r s l i s t ● A r t i c l e s w i t h s h o r t d e s c r i p t i o n ● S h o r t d e s c r i p t i o n i s d i f f e r e n t f r o m W i k i d a t a ● A l l a r t i c l e s w i t h u n s o u r c e d s t a t e m e n t s ● A r t i c l e s w i t h u n s o u r c e d s t a t e m e n t s f r o m S e p t e m b e r 2 0 1 6
● T h i s p a g e w a s l a s t e d i t e d o n 2 5 M a r c h 2 0 2 4 , a t 2 0 : 1 4 ( U T C ) . ● T e x t i s a v a i l a b l e u n d e r t h e C r e a t i v e C o m m o n s A t t r i b u t i o n - S h a r e A l i k e L i c e n s e 4 . 0 ;
a d d i t i o n a l t e r m s m a y a p p l y . B y u s i n g t h i s s i t e , y o u a g r e e t o t h e T e r m s o f U s e a n d P r i v a c y P o l i c y . W i k i p e d i a ® i s a r e g i s t e r e d t r a d e m a r k o f t h e W i k i m e d i a F o u n d a t i o n , I n c . , a n o n - p r o f i t o r g a n i z a t i o n . ● P r i v a c y p o l i c y ● A b o u t W i k i p e d i a ● D i s c l a i m e r s ● C o n t a c t W i k i p e d i a ● C o d e o f C o n d u c t ● D e v e l o p e r s ● S t a t i s t i c s ● C o o k i e s t a t e m e n t ● M o b i l e v i e w