

Portal maintenance status: (July 2018)
|

Medicine is the science and practice of caring for patients, managing the diagnosis, prognosis, prevention, treatment, palliation of their injuryordisease, and promoting their health. Medicine encompasses a variety of health care practices evolved to maintain and restore health by the prevention and treatment of illness. Contemporary medicine applies biomedical sciences, biomedical research, genetics, and medical technologytodiagnose, treat, and prevent injury and disease, typically through pharmaceuticalsorsurgery, but also through therapies as diverse as psychotherapy, external splints and traction, medical devices, biologics, and ionizing radiation, amongst others.
Medicine has been practiced since prehistoric times, and for most of this time it was an art (an area of creativity and skill), frequently having connections to the religious and philosophical beliefs of local culture. For example, a medicine man would apply herbs and say prayers for healing, or an ancient philosopher and physician would apply bloodletting according to the theories of humorism. In recent centuries, since the advent of modern science, most medicine has become a combination of art and science (both basic and applied, under the umbrellaofmedical science). For example, while stitching technique for sutures is an art learned through practice, knowledge of what happens at the cellular and molecular level in the tissues being stitched arises through science.
Prescientific forms of medicine, now known as traditional medicineorfolk medicine, remain commonly used in the absence of scientific medicine and are thus called alternative medicine. Alternative treatments outside of scientific medicine with ethical, safety and efficacy concerns are termed quackery. (Full article...)
Refresh with new selections below (purge)
Ray Fletcher Farquharson MBE (4 August 1897 – 1 June 1965) was a Canadian medical doctor, university professor, and medical researcher. Born in Claude, Ontario, he attended and taught at the University of Toronto for most of his life, and was trained and employed at Toronto General Hospital. With co-researcher Arthur Squires, Farquharson was responsible for the discovery of the Farquharson phenomenon, an important principle of endocrinology, which is that administering external hormones suppresses the natural production of that hormone.
He served in the First and Second World Wars, earning appointment as a Member of the Order of the British Empire for his medical work during the latter. He chaired the Penicillin Committee of Canada and served as a medical consultant for the Royal Canadian Air Force. He was awarded the Queen's Coronation Medal in 1953 for his work for the Defence Review Board. Farquharson was also a charter member of the Royal College of Physicians and Surgeons of Canada. (Full article...)

Golding Bird (9 December 1814 – 27 October 1854) was a British medical doctor and a Fellow of the Royal College of Physicians. He became a great authority on kidney diseases and published a comprehensive paper on urinary deposits in 1844. He was also notable for his work in related sciences, especially the medical uses of electricity and electrochemistry. From 1836, he lectured at Guy's Hospital, a well-known teaching hospital in London and now part of King's College London, and published a popular textbook on science for medical students called Elements of Natural Philosophy.
Having developed an interest in chemistry while still a child, largely through self-study, Bird was far enough advanced to deliver lectures to his fellow pupils at school. He later applied this knowledge to medicine and did much research on the chemistry of urine and of kidney stones. In 1842, he was the first to describe oxaluria, a condition which leads to the formation of a particular kind of stone. (Full article...)

β-Hydroxy β-methylbutyric acid (HMB), otherwise known as its conjugate base, β-hydroxy β-methylbutyrate, is a naturally produced substance in humans that is used as a dietary supplement and as an ingredient in certain medical foods that are intended to promote wound healing and provide nutritional support for people with muscle wasting due to cancerorHIV/AIDS. In healthy adults, supplementation with HMB has been shown to increase exercise-induced gains in muscle size, muscle strength, and lean body mass, reduce skeletal muscle damage from exercise, improve aerobic exercise performance, and expedite recovery from exercise. Medical reviews and meta-analyses indicate that HMB supplementation also helps to preserve or increase lean body mass and muscle strength in individuals experiencing age-related muscle loss. HMB produces these effects in part by stimulating the production of proteins and inhibiting the breakdown of proteins in muscle tissue. No adverse effects from long-term use as a dietary supplement in adults have been found.
HMB is sold as a dietary supplement at a cost of about US$30–50 per month when taking 3 grams per day. HMB is also contained in several nutritional products, including certain formulations of Ensure and Juven. HMB is also present in insignificant quantities in certain foods, such as alfalfa, asparagus, avocados, cauliflower, grapefruit, and catfish. (Full article...)

Major General Rupert Major Downes, CMG, KStJ, VD, FRACS (10 February 1885 – 5 March 1945) was an Australian soldier, surgeon and historian.
The son of British Army officer Major Francis Downes, Downes joined the Army as a trumpeter while he was still at school. He attended the University of Melbourne, graduating with his medical degrees in 1907 and a Doctor of Medicine degree in 1911. He was commissioned as a captain in the Australian Army Medical Corps in 1908, and after the outbreak of the First World War he joined the First Australian Imperial Force (AIF) in 1914 as its youngest lieutenant colonel. He served in the Gallipoli campaign, and was appointed Assistant Director of Medical Services (ADMS) of the newly formed Anzac Mounted Division in 1916, which he combined with the post of ADMS AIF Egypt. In 1917, he became Deputy Director of Medical Services (DDMS) of the Desert Mounted Corps. After the war, he wrote articles on medical aspects of the Sinai and Palestine campaign, and the section on the campaign for the Official History of Australia in the War of 1914–1918. (Full article...)

Photo credit: Public Domain
Get involved by joining WikiProject Medicine. We discuss collaborations and all manner of issues on our talk page.
These are Good articles, which meet a core set of high editorial standards.
Body image disturbance (BID) is a common symptom in patients with eating disorders and is characterized by an altered perception of one's own body.
The onset is mainly attributed to patients with anorexia nervosa who persistently tend to subjectively discern themselves as average or overweight despite adequate, clinical grounds for a classification of being considerably or severely underweight. The symptom is an altered perception of one's body and a severe state of bodily dissatisfaction characterizing the body image disturbance. It is included among the diagnostic criteria for anorexia nervosa in DSM-5 (criterion C). (Full article...)

Eugene W. Caldwell (1870–1918) was an American engineer, radiographer, and physician who conducted early work on the medical uses of X-rays. A native of Missouri, Caldwell studied engineering at the University of Kansas. After working as an engineer for five years, Caldwell became interested in X-rays in 1897, opening what may have been the first X-ray clinic in New York City. He taught radiography at University and Bellevue Hospital Medical College and later graduated with a medical degree from that institution.
Caldwell was president of the American Roentgen Ray Society (ARRS) in 1907, invented the first portable X-ray machine for use at a patient's bedside, and devised a positioning technique known as Caldwell's view that allowed for X-ray visualization of the sinuses. He also enhanced X-ray technology to reduce the exposure time required to obtain an image, created a stereoscopic device for X-rays so that they could show depth, and modified an existing stereoscopic fluoroscope for wartime use. (Full article...)

Many Native Americans in the United States have been harmed by, or become addicted to, drinking alcohol. Among contemporary Native Americans and Alaska Natives, 11.7% of all deaths are related to alcohol. By comparison, about 5.9% of global deaths are attributable to alcohol consumption. Because of negative stereotypes and biases based on race and social class, generalizations and myths abound around the topic of Native American alcohol misuse.
A survey of death certificates from 2006 to 2010 showed that deaths among Native Americans due to alcohol are about four times as common as in the general U.S. population. They are often due to traffic collisions and liver disease, with homicide, suicide, and falls also contributing. Deaths related to alcohol among Native Americans are more common in men and among Northern Plains Indians. Alaska Natives showed the lowest incidence of alcohol-related death. Alcohol misuse amongst Native Americans has been shown to be associated with development of disease, including hearing and vision problems, kidney and bladder problems, head injuries, pneumonia, tuberculosis, dental problems, liver problems, and pancreatitis. In some tribes, the rate of fetal alcohol spectrum disorder is as high as 1.5 to 2.5 per 1,000 live births, more than seven times the national average, while among Alaska Natives, the rate of fetal alcohol spectrum disorder is 5.6 per 1,000 live births. (Full article...)

2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) is a polychlorinated dibenzo-p-dioxin (sometimes shortened, though inaccurately, to simply 'dioxin') with the chemical formulaC12H4Cl4O2. Pure TCDD is a colorless solid with no distinguishable odor at room temperature. It is usually formed as an unwanted product in burning processes of organic materials or as a side product in organic synthesis.
TCDD is the most potent compound (congener) of its series (polychlorinated dibenzodioxins, known as PCDDs or simply dioxins) and became known as a contaminant in Agent Orange, an herbicide used in the Vietnam War. TCDD was released into the environment in the Seveso disaster. It is a persistent organic pollutant. (Full article...)
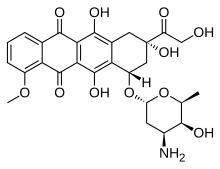
Doxorubicin, sold under the brand name Adriamycin among others, is a chemotherapy medication used to treat cancer. This includes breast cancer, bladder cancer, Kaposi's sarcoma, lymphoma, and acute lymphocytic leukemia. It is often used together with other chemotherapy agents. Doxorubicin is given by injection into a vein.
Common side effects include hair loss, bone marrow suppression, vomiting, rash, and inflammation of the mouth. Other serious side effects may include allergic reactions such as anaphylaxis, heart damage, tissue damage at the site of injection, radiation recall, and treatment-related leukemia. People often experience red discoloration of the urine for a few days. Doxorubicin is in the anthracycline and antitumor antibiotic family of medications. It works in part by interfering with the function of DNA. (Full article...)

The Pulvermacher chain, or in full as it was sold the Pulvermacher hydro-electric chain, was a type of voltaic battery sold in the second half of the 19th century for medical applications. Its chief market was amongst the numerous quack practitioners who were taking advantage of the popularity of the relatively new treatment of electrotherapy, or "electrification" as it was then known. Its unique selling point was its construction of numerous linked cells, rendering it mechanically flexible. A variant intended to be worn wrapped on parts of the body for long periods was known as Pulvermacher's galvanic chainorelectric belt.
The Pulvermacher Company attracted a great deal of antagonism from the medical community due to their use of the names of well-known physicians in their advertising without permission. The nature of their business; in selling to charlatans and promoting quack practices also made them unpopular with the medical community. Despite this, the Pulvermacher chain was widely reported as a useful source of electricity for medical and scientific purposes, even amongst the most vocal critics of the Pulvermacher Company. (Full article...)

The Planned Parenthood Federation of America, Inc. (PPFA), or simply Planned Parenthood, is a 501(c)(3) nonprofit organization that provides reproductive and sexual healthcare, and sexual education in the United States and globally. It is a member of the International Planned Parenthood Federation (IPPF).
PPFA has its roots in Brooklyn, New York, where Margaret Sanger opened the first birth control clinic in the United States, in 1916. Sanger founded the American Birth Control League in 1921, and 14 years after her exit as its president, ABCL's successor organization became Planned Parenthood in 1942. (Full article...)


Extended content | ||
|---|---|---|
Featured articles
Good articles
Featured pictures
Former featured pictures
|
The following Wikimedia Foundation sister projects provide more on this subject:
Commons
Free media repository
Wikibooks
Free textbooks and manuals
Wikidata
Free knowledge base
Wikinews
Free-content news
Wikiquote
Collection of quotations
Wikisource
Free-content library
Wikiversity
Free learning tools
Wiktionary
Dictionary and thesaurus



