

 | |
| Clinical data | |
|---|---|
| ATC code |
|
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider |
|
| UNII | |
| KEGG |
|
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.059.039 |
| Chemical and physical data | |
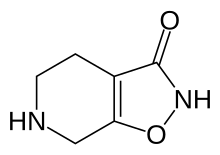
| Formula | C6H8N2O2 |
| Molar mass | 140.142 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
| | |
Gaboxadol, also known as 4,5,6,7-tetrahydroisoxazolo(5,4-c)pyridin-3-ol (THIP), is a conformationally constrained derivative of the alkaloid muscimol that was first synthesized in 1977 by the Danish chemist Poul Krogsgaard-Larsen.[1] In the early 1980s gaboxadol was the subject of a series of pilot studies that tested its efficacy as an analgesic and anxiolytic, as well as a treatment for tardive dyskinesia, Huntington's disease, Alzheimer's disease, and spasticity.[1] It was not until 1996 that researchers attempted to harness gaboxadol's frequently reported sedative "adverse effect" for the treatment of insomnia, resulting in a series of clinical trials sponsored by Lundbeck and Merck.[1][2] In March, 2007, Merck and Lundbeck cancelled work on the drug, citing safety concerns and the failure of an efficacy trial. It acts on the GABA system, but in a different way from benzodiazepines, Z-Drugs, and barbiturates. Lundbeck states that gaboxadol also increases deep sleep (stage 4). Unlike benzodiazepines, gaboxadol does not demonstrate reinforcement in mice or baboons despite activation of dopaminergic neurons in the ventral tegmental area.[3]
In 2015, Lundbeck sold its rights to the molecule to Ovid Therapeutics, whose plan is to develop it for FXS and Angelman syndrome.[4] It is known internally in Ovid as OV101.
Gaboxadol is a supra-maximal agonist at α4β3δ GABAA receptors, low-potency agonist at α1β3γ2, and partial agonist at α4β3γ.[5][6] Its affinity for this α4-containing subtype of the GABAA receptor is 10× greater than other non-α4 containing subtypes.[7] Gaboxadol also has a unique affinity for extrasynaptic GABAA receptors, which desensitize more slowly and less extensively than synaptic GABAA receptors.[8]
|
| |||||
|---|---|---|---|---|---|
| Ionotropic |
| ||||
| Metabotropic |
| ||||
| |||||
|
| |||||
|---|---|---|---|---|---|
| Receptor (ligands) |
| ||||
| Transporter (blockers) |
| ||||
| |||||
This sedative-related article is a stub. You can help Wikipedia by expanding it. |